“Could you come into my office for a moment?”
Three months after hearing these words from our pediatrician, the words still hurt to hear, and ring through my head in perfect clarity, like I just heard them 5 minutes ago. During an office visit where we were hoping to find out why our son was thirsty and peeing a little more at night, our Pediatrician brought us to his office to tell us that our son had Type 1 Diabetes (T1D).

Fatigue, drinking, and waking at night to pee, were telltale signs that something was off. 🙁
My eyes welled, and my back caved, and from that moment on it became very hard to hear anything that the doctor said afterwards, except those words that kept ringing in my head: Type 1 Diabetes. I knew that T1D can have a significant impact on a life, and has the potential to burden our son for the rest of his. What I did not know in that moment was everything else and what his illness would mean for him, for us, and what was next.
That is what this article is about: What comes next. There was, and still is, so much to learn about T1D, and I have since spent days on end trying to find and surround myself with the best resources available. My hope is that these resources become helpful for you and or others that you know as well.
1: Hospital Stay: Hydrate the Body and Reduce Glucose(Sugar) Levels in Blood with Insulin
“Why do I have to go to the hospital now? I’m fine. I want to go home” our son said.
Explaining to him at that moment that we needed to go to the hospital to do some testing and help take care of some high blood sugars that he had, did not stem his tears and it was clear to me that he knew that we were not going to escape this visit without many more tears, shots, fingerpricks, and heartache.
For anyone going through this diagnosis and early treatment, accepting Type 1 Diabetes and the complications and treatments offered by the medical team at this stage, is impossible for any patient or caregiver, and absorbing all of it really takes some time. Use your relaxation, or anti stress techniques here, and take heart in the fact that it gets easier from this impossible moment.
—
From here on, most people are likely to have slightly different experiences, depending on who their caregivers are and what the symptoms are that brought them to the doctor in the first place. Fortunately for us, we were very lucky on a number of fronts as we happen to be near a major Children’s Hospital with great doctors, and also our son did not have any significant symptoms that we could see were affecting him, and this is rare.
Many people are not so lucky and often bring their loved one to the doorstep of the hospital with severe symptoms of ketoacidosis that can be life threatening if left untreated.
—
Upon admission to the hospital, they drew blood and did a urinalysis again to confirm our pediatricians results. They also ran an A1C test to determine how affected his cells have been in the past 3 months. In our case he had an A1C level of 12.6. This level is considered by many to be very high, and most of the medical team that we saw were surprised that he was not experiencing more severe symptoms. A non-diabetic A1C is typically below 5.7.
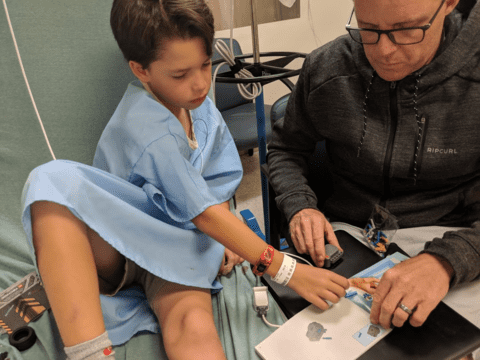
Next was the IV. Strangely, for someone who doesn’t spend a lot of time in the hospital, getting an IV can be very traumatic and scary. For my son this was probably the worst part of the experience for him and from the moment they put it in his small little hand, he was looking forward to getting it out.
The IV is critical though for delivering fluids and hydrating the body which is burdened by sugar. In our son’s case he had a Blood Sugar Level of 350 mg/dl, when normal for him should be below between 70-120. The extra sugar in his tissue dehydrates the body, and again the dehydration can be life threatening if untreated.
—
A Quick Primer on Diabetes
Diabetes is a condition where the body does not have the ability to bring glucose(sugar) into its cells, and an excess amount of sugar is carried in the body’s tissues and organs. Insulin is the special substance that allows sugars to be absorbed into the cells of your body and used for energy. In type 1 diabetes the problem is that the pancreas is not delivering enough insulin to the body and sugar builds, so the patient must supplement with external insulin. Basically the patient, caregivers, or new technologies must act as an artificial pancreas to supply insulin to the body, to keep it hydrated and out of a ketoaciditic state, and that’s where all the shots come in.
The good news is that this has been done for ~100 years and pharmaceutical insulin is well tolerated by the body and absolutely helps the sugar get into the cells to get converted into energy. The bad news is there has not been much in the way of progress on drug treatments with the exception of developing insulins that act quickly or slowly depending on the patients needs: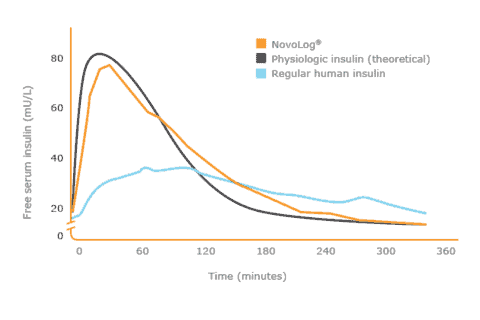
This chart shows the action cuve of Novolog (a commonly prescribed rapid acting insulin that is much closer to mimicking the action of Physiological insulin than the original “Regular” or R insulin.
If you would like more basic information on Diabetes or Type 1 Diabetes, my goto source for understanding the basics was Mayo Clinic’s website.
—
On the first day of our hospital stay, I began to understand a major reason we were there was to “stabilize” our son’s blood sugar levels and hydrate him, but I wasn’t sure what the requirement was for us to go home and I started to work toward that end, because none of us wanted to be there any longer than we needed to be. They kept saying that the earliest we can go home was likely 48 hours, so we began to focus on how we could make that happen.
The first thing that needed to happen was to get his blood sugar levels down and figure out how much insulin his body needs to keep his levels in a stable range. The doctors are most concerned at this point with him going too low with an excessive amount of insulin, so they will be hyper-vigilant about treating any low readings they see with sugar or carbohydrates. This is the reason for all of the finger sticking that goes on while you are in the hospital (don’t worry, you will not have to finger stick this frequently when you get home).
It wasn’t always clear why they cared so much about him going low, but I now understand that if left untreated an low can lead to a diabetic coma that has taken the lives of other children and T1D’s. Doctors can also be, and are often sued for allowing patients to become hypoglycemic and suffering any consequence that may occur in that event, so the doctors and hospitals spend a lot of time guarding against this possibility while you are in the hospital.
Managing T1D is not easily digested by patients or caregivers, and our visit was necessary for our education to begin and to learn the basics for what it takes to properly care for our son when we got home. As much as we wanted to leave, we were not educated enough to take care of his body yet and were also not mentally prepared for what comes next. There were many people at the hospital who offered helpful advice to us to get through those first couple of weeks at home, and while we don’t follow all the advice that was given to us there, on the whole they did a good job at stabilizing his glucose levels and transitioning us to understanding T1D and managing it at home.
I think for us, and for most people, the news of being diagnosed is shocking and if you are caring for a child during this time, you’re going to need help, because you are not yourself in these moments and your child needs the strength of people who are, around them. For the meantime, that strength can come from doctors and Hospital staff, and give you the time you need to grieve and work through your emotions. Do your best to surround yourself with friends and family who can give you a couple hours at a time to cry, rest, bond with friends, research, ask questions and get ready to go home. We did a lot of crying.
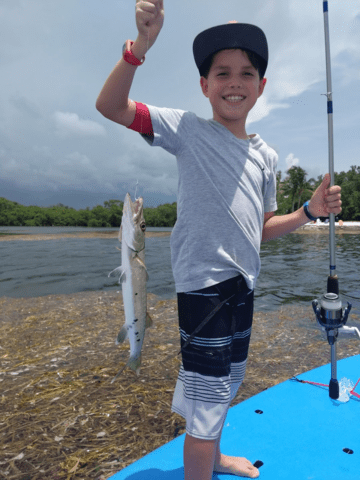
One incredible moment I had in all of this was seeing the strength that my 9 year old displayed as he received the load of bad news that the doctors kept consistently delivering to us, as they woke him to give him shots and stick his finger in the middle of the night, as they fed him hospital food and curtailed his meals, as he hugged and comforted us when he saw that we were sad, and as I watched him still rise above all of this and quickly transition to a laugh or happy mood at the drop of a joke or the suggestion to play a game. Looking back now, I realize that he was clearly living more in the moment than we were, and I can now see how powerful that can be to work through these tough days.
We were also very lucky to have a few of his friends stop by and breathe love into our room. To see him in those situations, with his friends was instantly heartwarming for me, and helped to reassure me that he was going to continue to have beautiful normal friendships.
What I wish someone would have told me at the hospital
Try to Live in the Moment as much as you can
This may sound trite, but do your best to stop trying to imagine the future, and what things are going to be like for you or your family member going forward. You are making yourself crazy, and I did. Look around, take some deep breaths and live in the moment.
You simply don’t have enough information to imagine what the future will look like while you are managing type 1 diabetes, and we needed at least 3 weeks worth of information before we had any idea, so take it day by day, hour by hour, and minute by minute. No one can predict the future anyway and the sooner that you work to live in the moment right now, the faster you will also become an effective caregiver that can handle this new challenge in all of your lives. There will be time for grieving, but for now, just try and listen, learn and live in the moment with your loved ones.
You are ok, and in the scheme of dramatic life changing events, you are going to survive this one and be fine. Yes, your life is changing, but I would put out there that life is always changing and requires you to be flexible to absorb these changes when they are presented. Patients and caregivers are all going through hell in this first 48 hours, so adding your worst fears about what the future might look like managing type 1 diabetes is not going to help anyone. They have made many advancements in the treatment and care for T1D that will make it much easier for diabetics to live complication free.
Just give it time and you will see quickly that with a little extra effort, you as a caregiver or a patient will be able to manage this disease successfully and lead beautiful lives together, and be afforded every opportunity that a non-diabetic would have.
Blood Glucose Level
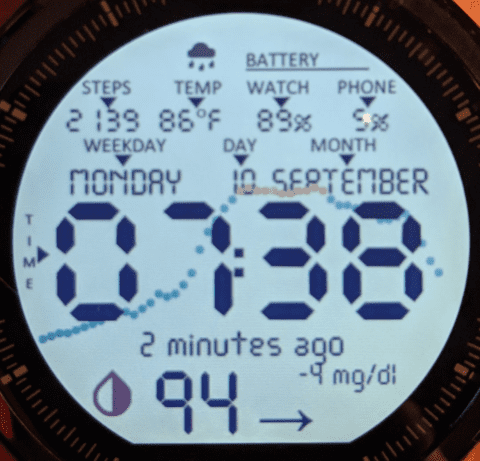
Going forward you will be wise to constantly monitor your patient’s blood glucose. The finger stick method that you learn in the hospital is important to know, but not how you will be measuring blood glucose on a daily basis after returning home and getting back to normal routines. This was the old way. Soon after leaving the hospital you will acquire a continuous glucose monitor (CGM) and use it to monitor your blood sugars on your phone, computer, or watch, at any time during the day, without finger sticking. So that should be a relief.
Here are the important points you need to know now in the hospital:
↓ Insulin is what brings blood sugar down
↑ Sugar is what brings blood sugar up
You are going to be assuming the role of the pancreas for the time being so it is good to know that the pancreas is responsible for regulating insulin in your body. Your goal is to learn how to keep your blood sugars in a safe range using injected insulin. You will learn a lot about how the body works when it is presented with different carbohydrates and sugars to do this effectively., and to avoid extreme high and low glucose readings.
Extreme Highs are dangerous and can dehydrate the body and introduce a state of ketoacidosis that requires immediate medical attention. Highs can be counteracted by using the insulin your doctor will prescribe..
Extreme Lows are dangerous, as not having enough sugar in your body can shut down your brain and can lead to coma or death if not treated immediately. Lows can avoided by supplementing with a predictable sugar tablet/gel/liquid (we use smarties and know that 1 smartie will bring his level up 10-15mg/dl). If a type 1 diabetic actually loses consciousness you will have a intravenous sugar shot( sometimes called a glucagon pen) that you can use to administer emergency glucose to the body when it cannot ingest it through the mouth.
There is not an agreed-upon number for these extreme highs and lows, and you will need to consult with your doctor, do your own research, and have some experience to know what these extreme levels are. Be sure to request this information while you are in the hospital, and know that over time these numbers may change as you integrate other methods for controlling blood sugar (diet and exercise).
Get A CGM As Quickly As Possible
In addition to learning how to manage blood sugar day to day, a big reason you are in the hospital right now is to learn to avoid these scenarios forever.
One thing I would recommend doing while you are in the hospital is to start working with the doctors and your insurance company to get a Continuous Glucose Monitor (CGM) as soon as possible. This is an invaluable tool that will give you a blood sugar reading every 5 minutes and will help you understand how the body is reacting to different foods and activities as you get back to your normal routines.
Figuring this out sooner than later will have benefits for you going forward that you will not understand until you have the data. You will feel much more knowledgeable about what is going on inside the body. These devices are not as expensive as you may think and if your hospital doctor will prescribe it you can always pay out of pocket to get a reader and sensor that is good for 10 to 14 days and it should not cost you much more than $150.
Insulin
You will leave the hospital with a basal insulin (long acting insulin) and a bolus insulin(rapid acting insulin). The basal insulin is meant to keep some level of insulin in your body at all times. The bolus insulin is meant to correct for meals and times where your blood sugar is high.
Diet
Don’t worry too much about this now, as you have plenty of other things to learn, but do keep in mind that regardless of what they tell you at the hospital that you can eat, when a type 1 Diabetic eats foods that contain grains, starches, sugars, or fruits, their blood sugar will go up, and they will need a proportionate amount of insulin to bring it down. Managing diabetes quickly becomes much easier when you learn to identify all the foods that contain these elements and that you now need to manage with insulin and reducing or eliminating these foods from your diet.
2: The Firehose: Researching Cures for Type 1 Diabetes and Saving Pancreatic Beta Cells
“When will the cure be available papa?” our son asked.
“I don’t know son, but there seem to be a lot of smart people out there who appear to be very close to finding a cure” I say with optimism.
On the first day of his diagnosis I went straight to the internet to find out all I could about cures and prevention strategies, hoping to find one. This is something I still do today but the lack of available cures for T1D worldwide has tempered my enthusiasm for this activity. Months of searching 100 years worth of of data on cures for T1D, has yielded nothing but opened or closed studies, and drugs that work on rats. Scientists have successfully cured diabetes in rats many times, but not in humans yet.
A cure would entail restoring pancreatic beta cell function for life, and rendering the autoimmune component of Type 1 Diabetes harmless, and there are some promising ongoing studies and new ones opening every month, but so far nothing you can ask your doctor for that will cure T1D in humans.
Months of research with no cure’s found for T1D, but lots of promising ongoing studies that will hopefully find a cure in the future..
Saving Pancreatic Beta Cells
As it becomes less likely that a recognized cure exists, we start to contend with the reality of having to inject insulin into my son four five times a day for the foreseeable future, and this is extremely hard for me to accept. No one likes giving or getting shots, especially our son, but I really don’t like injecting pharmaceuticals into my 9 year old who to date has been raised on organic foods and clean living. Every doctor, researcher, and parent at this point is giving us the same advice though, and that is to use insulin to keep blood sugar levels in range, and to rest the pancreas. So that is what we will do.
Still determined, and in lieu of a cure, my next idea is to find some way to save the beta cells in his pancreas and create an environment where the pancreatic cells that still exist today are able to function tomorrow and possibly grow new ones. Another way to say this is we are hoping to prolong or extend the honeymoon period indefinitely, so that if and when a cure does become available, his pancreas and body will be able to utilize it.
Prolonging the Honeymoon Period
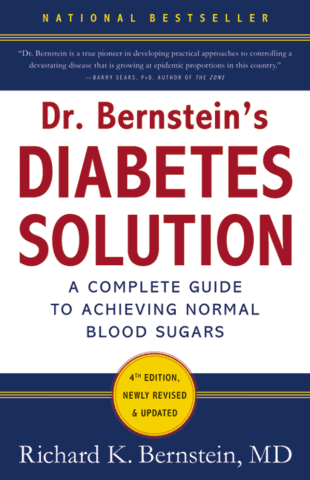
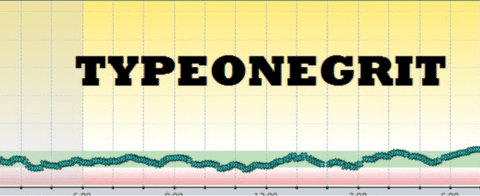
Dr. Bernstein and the incredibly knowledgeable advocates for a low carbohydrate approach in the Typeonegrit FB group, combine a low carb diet, with micro doses of insulin and measured micro doses of sugar, to control blood sugars in a very tight range. They believe, as many do, that with exquisite control of blood sugar, the honeymoon period can be extended indefinitely as there is really no pressure on the pancreas to perform.
“Based upon my experience with the fair number of type 1 diabetics I’ve treated from the time of diagnosis, I’m convinced that the honeymoon period can be prolonged indefinitely. The trick is to assist the pancreas and keep it as quiescent as possible. With the meticulous use of small doses of injected insulin and with the essential use of a very low carbohydrate diet, the remaining capacity of the pancreas, I believe, can be preserved.” – Dr. Bernstien The Diabetes Solution
 |  |
I also really like what Sonia Chritton had to say about prevention and extending the honeymoon period, and she has a website and facebook group where she talks more about her success using Vitamin D and Fish oil supplements to preserve beta cell function in people who are predisposed to, or recently diagnosed with T1D. She has slso been integral in developing the Poseidon protocol, a recent study which published some of the best thoughts around doses of supplements to take to reduce inflammation and preserve beta cell function.
Type 1 diabetes is an autoimmune disease and as such, it is a disease where the body attacks its own pancreatic beta-cells when they are working, and therefore visible to the body. So after taking all these great approaches into consideration, our thinking is that perhaps the next best thing to a cure is to try and decrease the amount of visibility that the pancreas beta cells have to the immune system, that wants to attack them.
By combining some of the approaches above to managing T1D, facilitating an environment in the body for healing, and working to prevent further damage to the body, we are now dedicated to maintaining normal blood sugars, taking pressure off the pancreas, and reducing inflammation.
Diet and Insulin
There is a Grand Canyon of disagreement between the American Diabetes Association guidelines for managing diabetes with diet and insulin, and the progressive approach of a growing group of people worldwide who believe that diabetics should be entitled to, and aiming for having normal blood sugar levels.
The American Diabetes Association would suggest that having an A1C of 7.0 is a reasonable and admirable A1c. This is nowhere near normal for most people (normal blood sugars for non diabetics are around 4.5). People who have A1C’s above 6 often show markedly increases risk for nearly all the long term complications of diabetes. So why you may not see complications immediately from these higher blood sugar numbers, in the future you can almost be guaranteed of one or many typical complications of diabetes if you let your blood sugars run this high.
While desirable, achieving normal blood sugars up until now, has not been easy This group of progressives has been pretty small until lately,and is now growing exponentially as new tools emerge for monitoring (CGM’s), and more research reveals the benefits of low carb eating(ever heard of Keto?), which make it much easier to see and to maintain stable blood sugars.
You will need time to do your own research and find out which path and guidelines you want to follow when you get home, but for us and many of the recently diagnosed, it comes down to this choice:
- Follow the status quo ADA Guidelines
- Larger inputs of carbohydrates (“Eat what you normally eat)
- Larger inputs of insulin
- Higher Blood Sugars and A1C
- Big Swings in Blood Glucose Levels
- Higher Pancreas Demands
- Shorter Honeymoon Period
- Greater number of Typical Lifetime Diabetic Complications
- Subtle to no modifications of diet
Typical Blood Glucose Levels Using ADA protocols and a High Carb Diet: A1C 7.0 or 154mg/dl
Or
- Follow the Normal Blood Sugar Advocates
- Small inputs of carbohydrates
- Small inputs of insulin
- More Normal Blood Sugars and A1C
- Small Swings in Blood Glucose Levels
- Low Pancreas Demands
- Smaller number of Typical Lifetime Diabetic Complications
- Major shift in diet to a Lower Carb model of eating
Study in Pediatrics JournalDr. Berstein’s Diabetes University on YoutubeDiabetes SolutionType One Grit Facebook Group
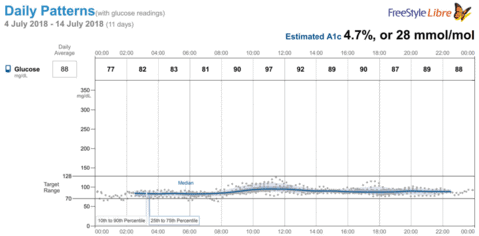
Progressive blood Glucose Levels Using Low Carb protocols and diet: A1C 4.5 or 83 mg/dl
From the bias in this writing I’m sure you can tell that we chose the guidelines in path number two – following a more progressive approach to normalizing his blood sugars so that he truly will not be affected by having high blood sugars in his body, and can avoid having diabetic complications all together.
Supplements
“I love pills” our son said.
Wait, what?
“Yes I love taking pills.”

Supplements for reducing inflammation, balancing the immune system, and protecting beta cells
That’s really what he said. I know everyone isn’t going to be this lucky, but for right now he is okay with taking 7 supplements a day.
There are likely to be a lot of opinions on which supplements to take so I’m not going to go into too much detail on the ones we use, but we are very interested in the research that Doctor Ricordi is doing in the Poseidon study, with vitamin D and DHA fish oil.
We have been following his protocol with Vitamin D and DHA dosages fairly closely and are about to test our levels to see where we’re at with vitamin D and DHA in the blood, using the test supplied at Grassroots health.
We don’t have a lot to compare our results to because we started taking these supplements right after we got home, but something seems to be working because our insulin dosages are still going down and he is gaining weight and height at a rapid pace, so we will stick with it and continue to keep track of Dr Ricordi, and Sonia Chritton’s work
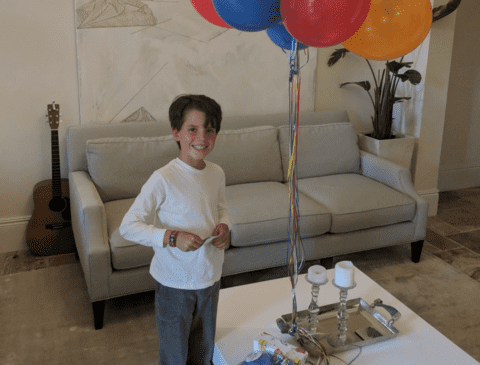
3: Family Life and Getting Back to Normal
Getting home and those first nights
It was so nice to get back to our home and see some of our normal sights after being in the hospital for 48 hours. It was equally painful, I remember, thinking about all of the foods that were going to be difficult for him to eat, and knowing that I had to sort through the pile of syringes, glucose test strips, lancets, insulins, and alcohol swabs, etc., and find a way for them to get integrated into our lives. It was bitter sweet.
We called the doctor a lot in those first few weeks to verify what we learned in the hospital and of course the whole experience created a lot of uncertainty and tension in our home. it really does take a month or so to begin to understand what this disease will mean to you and your family going forward but take heart that the tools available today are making it infinitely easier to manage and will only likely improve from here.
The night times were scary because of our experience at the hospital and their insistence on waking him up at night to measure his blood sugar level. Figuring out what to do at 3 in the morning when you are exhausted emotionally and physically is also a challenge but you make it work because there is no alternative.
It is very important, and the hospital makes clear that you do not want to find yourself in a hypoglycemic event situation. They encourage you to aim for higher blood glucose to start out so that if you do end up with too much insulin, or your blood sugar begins to drop, you will still have some room to go before it gets critically low.
With the help of continuous glucose monitoring, you will start to get some sleep again as the device will wake you up with alarms if his levels begin to go too low, and you can set the thresholds for your comfort levels.
Okay, now that we have got a night or two under our belts, it’s time to figure out what we’re going to eat. Off to try and find some low carbohydrate foods.
Foods
I thought we were going to rejoice in going to our favorite grocery store Trader Joe’s, or our local grocery store chain Publix, to find a plethora of low carbohydrate foods to select from. Ah….no. To our dismay almost all of the pre-packaged foods had greater than 20 grams per serving of carbohydrates in them. After studying labels for hours it is clear that about ¾ of grocery store items, are laden with too many carbohydrates to be integrated into a low carb diet.
Amazon Fresh to the rescue. In addition to being a more pleasurable low carb shopping experience, we found that we can find almost everything that we need on their site and much of it is reasonably priced. It’s a beautiful sight to see groceries on your doorstep in the morning and know that you don’t need to make a special trip to three stores to find everything you need.
So how do you switch your 9 year old from eating a typical American high carb diet to eating a low-carb diet? With the help of people who have already done it. RD dikeman at type 1 Grit, Carolyn Ketchum at “All day I dream about food”, and a few other internet resources proved to be particularly helpful. They have been there and done this, and have many published resources with delicious substitute recipes for almost every food imaginable including pastas, desserts, and pizzas! Here is a page with our favorites.
When our son found out that he could eat ice cream and pizza, without significant spikes in blood sugar, he was so relieved and started to be interested in these new versions of familiar foods. He actually started to fancy himself as a food critic, suggesting modifications to suit his tastes. He is a champ, and once he realized that there were still a ton of great foods that he enjoyed eating, making the switch to this new low carb, high protein, higher fat diet was actually pretty easy for him.
For us, the challenge has become to be sure he continues to gain weight, continues to grow, eats plenty of protein and healthy fats, eats plenty of greens and vegetables, and feels included at all meals whether they are at home, out, at school, or at friends.
Going out
For being such a healthy eater at home, it’s amazing how many times we used to go out and he would order a hamburger. Fortunately there is an excellent hamburger bun recipe that you can use to make buns to take when you go out, and you can freeze as many of them as you need so you always have a supply. Substitute a side of vegetables for french fries and use a very small amount of ketchup and this is an easy way to go to most restaurants. He has also taken a liking to blackened fish, and salads at chipotle.
We still have some work to do here, but this has been a good start for us, and there are some great resources available as well. Here is a funny one about fast food restaurants and what to order.
School
Fortunately for us, our school has been amazing in working our son to help him manage his T1D throughout the day. Basically he stops in the nurses office right before lunch and any time he feels off, low, or if he needs a snack. The nurses require a management plan to follow from his endocrinologist and we keep a kit of supplies and an extra glucagon kit there in case of an emergency where his blood sugar goes too low.
What was less great was the amount of sugar being handed out on a regular basis in the classroom. We are in the process of working with the school to create a wellness policy that will this issue and create a healthy environment for all kids. Here is a copy of the petition we started to get the school to take note of this issue.
Friend Visits
It’s incredible to see how our friends have embraced our family’s new diet and have challenged themselves to find low carb foods to serve at their homes when we visit. We typically pack enough food for a meal and a snack for him just in case, but almost always find enough protein and vegetables where ever we go.
My wife and I try to bring desserts for our friends and their kids, and will bake low carb cookies, lemon bars, and we even made ice cream at one party. The kids love it, and they are all amazed when they find out there is no sugar in the delicious desserts they are consuming. Best of all, our son gets to enjoy being included and also appreciated during dessert time and that goes a long way for us and this age.
Tools
CGM
The continuous glucose monitor is a complete revolution in diabetes monitoring and care, and Is changing the way that people are able to manage and care for diabetes. In the past you would need to finger stick 10 times to get 10 readings during the day and try and decipher from those readings what foods and activities did to your blood sugars.
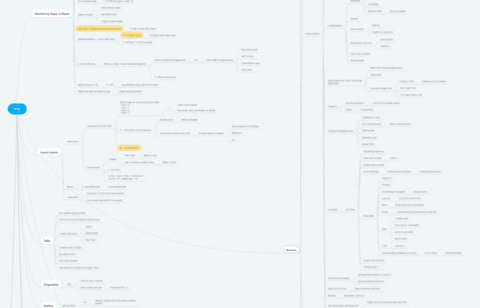
Now, with a continuous glucose monitor that gives readings every 5 minutes you will get a total of 288 readings per day that you can evaluate in a graph like the one below. Armed with this information, you can make decisions about what and when to eat, the timing of your insulins, the amount of insulin needed, and note any patterns in the way your blood glucose levels fluctuate over time. Also important is their ability to trigger alerts when your blood sugar gets too low, or too high and allows you to take action quickly before a real problem would arise.
There is other information that you can begin to see in these levels and I believe that this will be a popular monitoring and feedback tool for anyone who wants to stay healthy.
We started off with a freestyle Libre as we could purchase it out of pocket for about $150 including a sensor. Each sensor cost about $30 and now how they work up to 14 days before having to replace the sensor. the freestyle Libre needs and NFC Reader to read the blood sugar levels off of the sensors period a clever few companies have built piggyback devices that sit on top of the sensor, reading it every 5 minutes or so, and delivering the reading via Bluetooth to a collecting cell phone or watch. The device that we found to work the best is called a miaomiao.

Installing the sensor is very straightforward but certainly intimidating for the caregiver and the patient and I would recommend one of the good YouTube videos of kids getting the sensor installed, so that you can see how easy and harmless it is.
When our insurance kicked in and delivered our prescribed CGM, 45 days after our hospital stay, we received the Dexcom system pictured below. It works a little bit differently then the Freestyle Libre in that it broadcasts blood sugar readings every 5 minutes over Bluetooth out of the box, and does not require an NFC Reader to get close to the sensor and read the levels. A phone or bluetooth reader placed within 100 feet of the Dexcom sensor should be able to pick up the readings and deliver them to the cloud and then to any device you choose as a reader.
Though they both work a little differently, and provide slightly different conveniences, their real value is in their ability to show you exactly what is happening with your blood sugar at any moment in time. This is what is going to allow you to tightly control your diabetes and give your loved one a chance at a complication free lifetime.
Insulin
This is still my least favorite part of diabetes and I’m sure it is my son’s as well. In the beginning we were trying to keep the dosages and the frequency of shots low, and we did actually get down to some very low dosages (about 6x less than what they prescribed us at the hospital) . But soon we realized that it was more important to be aiming for normal blood sugars and being sure that our son was getting enough food to keep him growing and energized, than to worry about the number of shots he was getting or having some low dosage. Fortunately for us, with a low carb diet, and our current diabetes management, we got both and he is maintaining normal blood sugars and using small bits of insulin while eating an extremely healthy low carb diet.
He still shrieks in pain occasionally when the shot hits a nerve, and bruises sometimes when getting the shot, but he has been incredibly brave about his regimen of getting 4 shots a day and does not miss a beat whether the shots go in easy or they hurt.
A note about needles and sizing:We started off using pens that had 4 mm needles on them and that were extremely thin. Unfortunately the pens would not give accurate delivery for us in 1/2 and 1 unit dosages(looking forward to the day when this changes), so we needed to switch to syringes and the syringes are only made in 6 mm needles. That is actually a pretty big needle for a nine-year-old that doesn’t have much fat on his body at all, but we have no choice.
 |  |
Watches and Phones
“I get a phone? and a smartwatch?”
Yes you do.
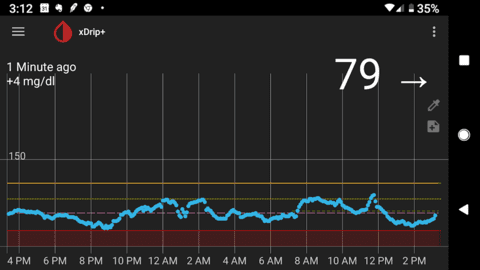
This is a screenshot of the open source app called xdrip that tracks and manages blood glucose readings
If there is a silver lining for a 9-year-old boy to being told that he’s going to have to have a multitude of shots every day and he really shouldn’t eat sugar for the foreseeable future, getting a phone and a smartwatch is a great privilege for someone his age, and helps to bring a few extra smiles to his days when he gets to tell his friends.
We are the parents that had planned not to give our child a phone until they really needed it, but it is simply too valuable of a tool not to have, so we work to give him a few freedoms with it but still maintain strict control over when and where he can use it.
The amazing thing about using these tools with a CGM Sensor is that when he carries it with him, or if it is within a hundred feet of him, his blood sugar readings are captured by the phone every 5 mins and he can view them at any time. Alarms can also be set to thresholds that allow for notifications when he goes too high or too low. Thanks to the internet, his blood sugars are also now distributed to us wherever we are, and we can communicate with him to help him manage his blood sugars with insulin, snacks, or sugar. It’s really pretty amazing considering just 3 years ago none of this was possible. Sensors and wearable technology have come a long way since then and we are lucky to be taking full advantage of these new technologies.
Ozone
“Ozone also appears to enhance the activity of cellular metabolism, the continual conversion of food into energy. Dr. Shallenberger likens the metabolism-heightening effect of ozone to a similar benefit to diabetics obtained through vigorous exercise. It oxygenates the tissues and gets all the body processes running better, he says.
Levels of ATP, an important molecule which stores energy in the cells, are also enhanced through ozonation. Among other functions, ATP helps each cell maintain the integrity of its membrane, thereby enabling it to regulate the passage of materials into and out of the cell.” says Dr. Shallenberger.
We have some experience with ozone from dealing with another autoimmune disease in our family when my wife contracted Lyme disease and the only solution that worked for her was doing ozone therapy on her blood at home. At that time we purchased an ozone machine and oxygen tank, and supplied ozone gas to her blood a couple times a week, and slowly she emerged from a 4-year battle with the autoimmune disease in excellent health.
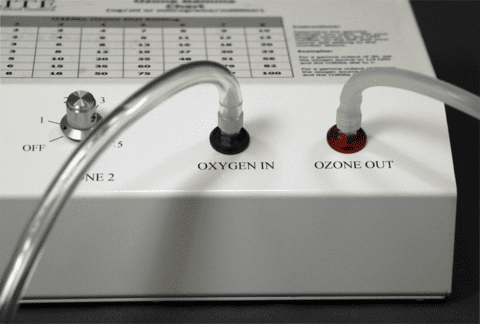
This is the machine we use. We purchased it to treat lyme disease but are starting to use it for T1D
If you search Ozone Therapy on the internet you will find a few experts like Dr. Rowan, Dr. Shallenberger, Dr Mendez, and Dr. Robbins. You will be unlikely to find anybody who says that ozone can cure diabetes, but you will find many cases where ozone helps to restore oxygen to tissue that is oxygen-depleted.
We were very slow to integrate this into our daily regimen but 4 months after diagnosis we are introducing it slowly and seeing some hopeful results. More on that in another upcoming post.
I have not been able to find many articles or practitioners using ozone to treat or cure diabetes but there are a few quotes out there that got my attention like the one above.
4: The Future and our Hopes and Dreams
That brings us to where we are today and our hopes and dreams for him. We want him to enjoy his family, friends, education, activities and to never feel limited or excluded because of T1D.
We continue to enable him with tools to take responsibility for his health and diet as we all continue to scan the horizon for treatments and therapies that hopefully will one day cure his T1D.
Hopefully this work will lead him to a complication free lifetime of excellent health, with normal blood sugars, while preserving as much pancreatic beta cell function as possible, so when a cure does present itself he will be able to take full advantage of it.
So far so good.
 |  |
 |  |